A team of researchers at West Virginia University recently developed artificial intelligence models that can diagnose heart failure using data from low-cost electrocardiograms, offering a potential breakthrough for patients who don’t have access to expensive medical treatment.
Heart failure is one of the most critical issues worldwide and its effects are especially severe in rural regions like Appalachia.
The study, published by Scientific Reports, addresses a critical gap: most AI systems for cardiac diagnosis are trained on data from patients in large urban hospitals. This marginalizes rural communities where lifestyles, environmental factors and access to care differ.In a press release from WVU Today, Prashnna Gyawali, an assistant professor at WVU, gave an example of someone in a rural area who may experience heart failure.
“She has limited access to specialty care, relies on a small local clinic, and her lifestyle, diet and health history reflect the realities of her environment: high physical labor, minimal preventive care, and increased exposure to environmental risk factors like coal dust or poor air quality,” Gyawali said.
To tackle the issue and build a system for people in rural areas, the team analyzed medical records from 55,500 patients across 28 hospitals in West Virginia.
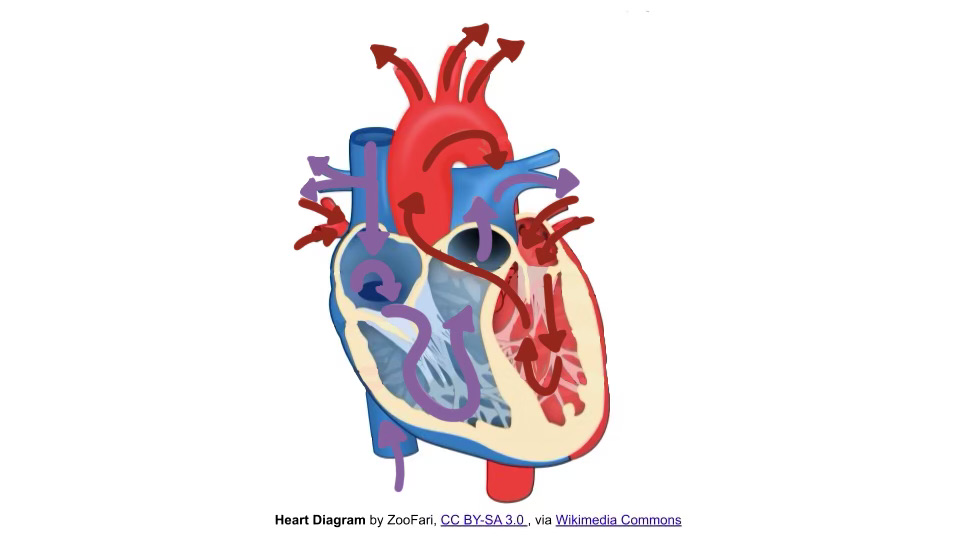
Unlike the echocardiogram, the current “gold standard” for measuring ejection fraction is a key indicator of heart function.
ECGs are relatively cheaper, quick and widely available. The challenge was whether AI could learn to predict ejection fraction accurately from ECG signals alone.
“Ejection fraction” is the percentage of blood pushed out of the heart with each beat. Low numbers signal the heart is struggling.
Researchers tested a wide range of models, from older methods like support vector machines and random forests, to advanced deep learning approaches, including transformers and Residual Network neural networks.
Their findings were striking: deep learning models were already much better at identifying when the heart wasn’t pumping enough blood, accurately identifying healthy and unhealthy patients.
“Echocardiography is expensive, time-consuming and often unavailable to patients in the very same Appalachian states that have the highest prevalence of heart failure,” Alina Devkota, a doctoral student, said. “They do have access to inexpensive electrocardiograms, so we tested whether AI models could use electrocardiogram readings to predict a patient’s ejection fraction.”
The research also highlighted how different ECG leads contributed to accuracy. A single reading wasn’t enough to predict heart failure on its own, however, certain combinations of signals made AI much better at finding problems.
The researchers demonstrated that the system was picking up on real patterns in the heartbeat that doctors already use when diagnosing patterns, rather than simply making random guesses.
These results reveal the impact of AI in expanding access to cardiac care in rural areas. West Virginia ranks first in the U.S. for the prevalence of heart attacks and coronary heart disease. However, many residents lack access to echocardiography.
An AI tool that works with ECGs could bridge that gap and allow early detection, potentially saving lives.
The researchers warned that it would take more work, and their dataset was limited to West Virginia.
Future studies are needed to test the models on patients from other regions to ensure the technology is reliable.
Deep learning models also demand large amounts of data, so collaboration across hospitals and states would be necessary to build stronger systems.
“Approximately 1 in 4 people alive today will experience heart failure during their lifetimes,” Gyawali said.
“The prevalence is even higher in rural Appalachia, so it’s critical the people here do not continue to be overlooked.”