New research from Boston University suggests that microplastics can reinforce the growth of antibiotic-resistant bacteria.
Bacteria are small, single-celled organisms that can reproduce without a host. Most are harmless; however, bacteria can also lead to a variety of illnesses, like tuberculosis. Therefore, antibiotics are a class of drugs used to kill bacteria, such as penicillin, or prevent their replication, like tetracycline in acne cream.
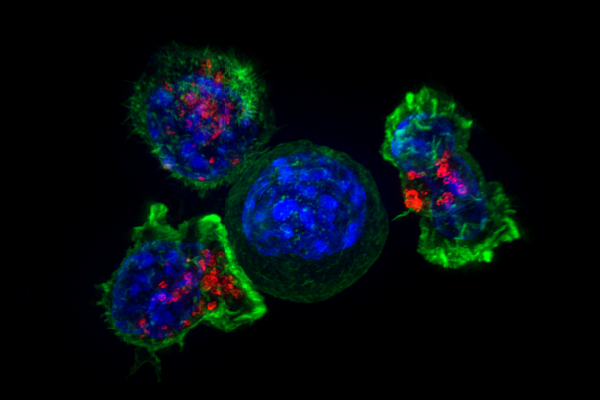
However, bacteria can develop resistance to antibiotics, making the treatments less effective. One way is through natural selection, where only antibiotic-resistant bacteria survive to reproduce. Alternatively, bacteria can also share genetic material with each other if they are close enough. To stay close to each other, bacteria like to form slimy groups called biofilm surfaces.
In addition to being generally disgusting, biofilms offer bacteria a fantastic chance to socialize and share helpful genes with their neighbors. If an antibiotic is introduced, the bacteria can quickly adapt and become antibiotic-resistant. This is very good for bacteria, and very bad for people who get infected by it.
Bacteria are always in search of new surfaces to colonize by forming biofilms. One promising home for any self-respecting bacteria colony is a floating microplastic. Microplastics are small pieces of plastic less than five millimeters thick. Microplastics, like bacteria, are all around. They’re commonly given off by car tires, synthetic clothing and plastic bottles. Bacteria love to form films on their surfaces and travel around with the plastic.
Just as concerning, microplastics are known to absorb antibiotics and prevent them from reaching the targeted bacteria.
The study aimed to examine the interplay between microplastics, bacteria and antibiotics. Researchers added differing quantities of microplastics to plates containing cultures of E. coli. The bacteria proceeded to form biofilms on the microplastics. Then, the scientists swirled the solution to free the bacteria from the microplastics and deposited them onto new plates.
These plates were either uncoated or coated with microplastics, antibiotics or both. The researchers used four common antibiotics: ampicillin, ciprofloxacin, doxycycline and streptomycin.
Bacteria were then allowed to grow for 10 days. The researchers found that the combination of microplastics and antibiotics led to selection for bacteria that attached themselves to the biofilm. Further, the mere presence of microplastics led to hugely increased survival rates: for instance, a colony treated with ciprofloxacin and just 0.005 millimeters of microplastics had more than eight times as many bacteria as a colony without microplastics.
The combination of microplastics and antibiotics led to the growth of an antibiotic-resistant colony that clung tightly to the ball of microplastics. These small balls can travel around, spreading the resistant bacteria wherever the microplastics go.
The potential impact of roving drug-immune bacteria on ecosystems and human population could be devastating. Microplastics are a more pressing issue than ever before, as both a contaminant and disease vector.