In a recent study published in Science Advances, scientists at the University of Connecticut have identified a previously underappreciated mechanism that may contribute to the onset and progression of neurodegenerative diseases such as Alzheimer’s disease, Amyotrophic Lateral Sclerosis and frontotemporal dementia.
At the center of this discovery is the protein TDP-43, long known for its role inside neurons, now shown to compromise the brain’s vascular integrity as well.
TDP-43 is widely studied in the context of abnormal protein clumping within neurons, a hallmark of several brain diseases. However, this new work reveals that TDP-43 also plays a crucial role in maintaining the blood-brain barrier, or BBB, a tightly regulated interface that shields the brain from harmful toxins and inflammation.
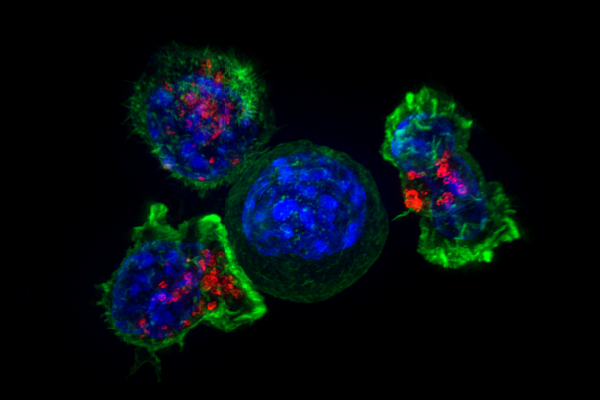
When levels of TDP-43 fall in the endothelial cells lining blood vessels, the BBB begins to deteriorate, allowing pro-inflammatory molecules and immune cells to enter the brain.
To investigate this mechanism, researchers used multiple genetically engineered mouse models, including one carrying a TARDBP mutation associated with ALS and another with endothelial-specific deletion of TDP-43.
In both cases, the animals exhibited increased blood-brain barrier permeability, inflammation and behavioral changes resembling cognitive and motor impairment.
These results suggest that vascular dysfunction may not simply be a downstream consequence of neurodegeneration; it could instead be an early and potentially initiating factor.
Additionally, the study raises the possibility that dysfunctional endothelial cells might contribute to disease spread. The researchers found that TDP-43 pathology in vascular cells could potentially propagate to neighboring neurons and glial cells, amplifying damage across different cell types.
This mechanism may help explain the widespread distribution of TDP-43 inclusions observed in postmortem brain tissue from patients with neurodegenerative disorders.
These findings have meaningful implications for the future of therapeutic development. If vascular dysfunction precedes neuronal loss, strategies aimed at preserving blood-brain barrier integrity, such as stabilizing TDP-43 function in endothelial cells, could delay or even prevent disease onset.
However, the underlying causes of TDP-43 dysfunction remain elusive.
While rare genetic mutations in the TARDBP gene have been linked to familial cases of ALS and frontotemporal dementia, the vast majority of patients do not carry these mutations. Yet, in nearly all of them, the TDP-43 protein still becomes mislocalized, aggregated or otherwise dysfunctional.
This disconnect raises a critical question: What else is going wrong?
“While some people with ALS or frontotemporal dementia carry mutations in the TDP-43 protein, most patients do not — yet the protein still becomes dysfunctional in nearly all cases,” co-lead author Dr. Ashok Cheemala said. “This tells us that other unknown factors in the body might be causing TDP-43 dysfunction.”
Those factors could include chronic inflammation, vascular stress, metabolic imbalance or environmental exposures, any of which might push an otherwise normal protein past its breaking point.
Identifying these triggers could unlock entirely new strategies for preventing or halting neurodegenerative disease, even in patients with no known genetic predisposition. For now, the hunt continues to uncover why TDP-43 goes rogue and how to stop it before it starts causing damage.
Ultimately, this research challenges the neuron-centric view of neurodegeneration. It suggests that the BBB is not merely a passive wall but an active participant in brain health, and it is potentially one of the earliest battlegrounds in the fight against Alzheimer’s, ALS and related conditions.