In a recent study published in Nature Metabolism, scientists at Baylor College of Medicine uncovered a surprising link between motion sickness and obesity.
While the classic image of motion sickness is someone feeling queasy or nauseous on a bumpy bus ride, the researchers found that the very brain circuitry that triggers the uncomfortable churn may also dial down (or up) our metabolic balance, potentially influencing body weight over time.
Using a new mouse model of motion sickness, the team, led by principal investigator Yong Xu, Ph.D., and postdoctoral fellow Longlong Tu, Ph.D., zoomed in on a region of the brain called the parvocellular part of the Medial Vestibular nucleus.
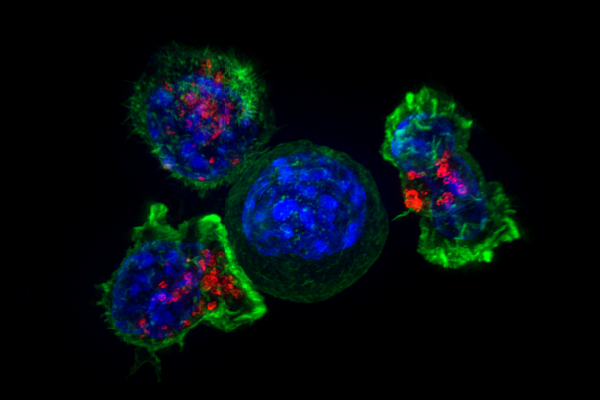
By placing mice on a mild “rocking” platform, they noticed a stark drop in the animals’ body temperature – similar to the chills a person may feel during motion sickness.
Moreover, they discovered that a specific subset of MVePC neurons, when artificially stimulated, perfectly reproduced these symptoms on demand, including a surprising shift in the mice’s ability to maintain a healthy weight.
According to the accompanying research briefing written by the lead authors, these MVePC neurons are mostly glutamatergic, meaning they are excitatory, and they form a circuit with a downstream brain region known as the Lateral Parabrachial Nucleus.
When the researchers inhibited the MVePC-LPBN circuit, there was a significant reduction in motion-induced hypothermia, while other brain functions were left unaffected.
The authors noted in the briefing: “We have identified the neural substrate of motion-induced hypothermia in mice as projections of MVePCGlu neurons to the LPBN,” they said. “We have also provided direct evidence that scopolamine targets these vestibular neurons to ameliorate motion-induced hypothermia.”
This suggests that existing medications such as scopolamine (a muscle relaxant used to treat postoperative emesis, or vomiting) may be particularly effective at treating motion sickness across multiple patient populations.
Even more intriguing, the team saw that chronically dampening these “motion-sensitive” neurons could help prevent diet-induced obesity without forcing the animals to eat less.
To elaborate, when they selectively silenced MVePCGlu neurons in mice, the animals stayed leaner despite consuming the same number of calories as their peers.
In other words, these neurons don’t just mediate whether you feel nauseous; they also appear to affect energy expenditure and metabolism within the entire body.
“When Longlong Tu, PhD, a postdoctoral fellow in my lab, proposed to investigate the brain circuits involved in motion sickness, a condition for which he is highly susceptible, I was not very excited about the idea because it’s not one of the main interests of my lab,” Dr. Xu said in an interview with GEN.
“However, I became more interested and supported Tu’s idea when he explained the emerging evidence suggesting a link between motion sickness and metabolic balance, which is one of my research interests.”
The implications for this research extend beyond assisting those with nausea. If the same neurons that spur motion sickness can alter thermoregulation and metabolism, then, as Drs. Tu and Xu suggest, “…better regimens for motion sickness treatment might specifically target vestibular neurons.”
In turn, subtle tweaks to this circuit could also become a new strategy for combating obesity – particularly one that doesn’t focus solely on appetite suppression or drastic dietary changes.