A new study by researchers at University of California San Diego has provided insights into why men and women experience and respond to pain treatments differently. Led by Dr. Fadel Zeidan, a professor of anesthesiology at UCSD and an endowed professor in empathy and compassion research, the study highlights that men and women use distinct biological pathways for pain relief during meditation. The findings have profound implications for understanding addiction risks and developing sex-specific pain therapies that could improve outcomes for both men and women.
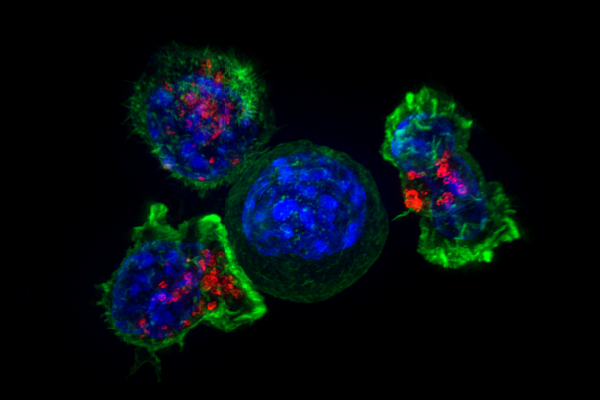
The study’s results reveal a fundamental difference in how each sex biologically process pain, which could help explain why certain treatments work better for some individuals than others. The researchers discovered that men typically depend on the endogenous opioid system for pain relief.
This system, which is naturally produced in the body, releases chemicals that activate receptors in the brain, reducing pain and promoting feelings of relaxation. Opioid-based medications, such as morphine and fentanyl, work by tapping into this system, allowing synthetic molecules to bind to the same receptors and create powerful pain-relieving effects.
When the researchers administered naloxone, a drug that blocks both synthetic and endogenous opioids, meditation-based pain relief in men ceased. Women, however, showed a different response: meditation continued to relieve pain in women even when the opioid system was blocked with naloxone, indicating that women rely on a separate, non-opioid pathway for pain relief.
“Men and women both have significant pain relief through meditation, but the pathways to that relief differ,” Zeidan said. “The study provides clear evidence of sex-based differences in pain processing, highlighting a need to take these differences more seriously when developing pain treatments.”
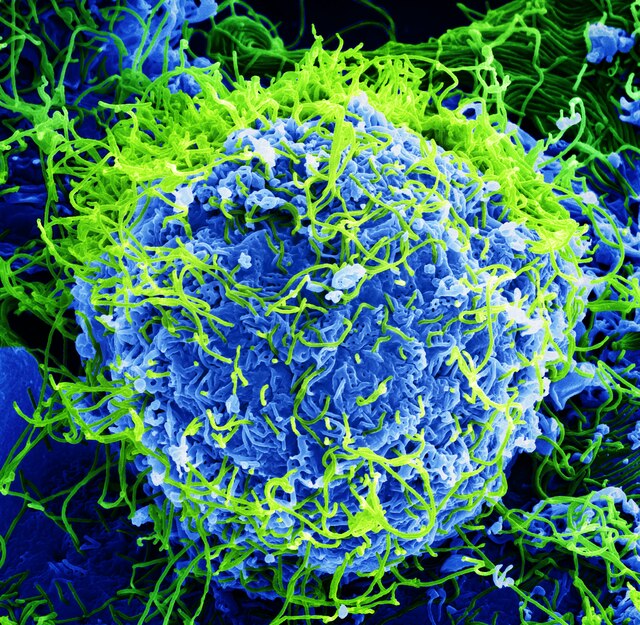
The study’s findings on the mechanisms behind pain relief could also shed light on the greater addiction risks associated with opioid use in women. Women are known to experience chronic pain more frequently than men and often report lower levels of relief from opioid-based painkillers. This inefficacy may drive some women to increase their opioid dosages in an attempt to achieve adequate relief, potentially leading to addiction.
“Dependence develops because people start taking more opioids when their original dosage stops working,” Zeidan said. “Although speculative, our findings suggest that one reason women are more likely to become addicted to opioids is that they’re biologically less responsive to them and need to take more to experience any pain relief.”
The research highlights an urgent need to develop alternative pain management therapies that don’t rely solely on opioid-based systems, particularly for women. As opioid misuse and overdose rates continue to rise, understanding these underlying biological differences could lead to safer, more effective pain treatments and help mitigate addiction risks for both sexes.
These findings advocate for a more tailored approach to pain management, where treatments align more closely with each sex’s unique biological mechanisms. Many pain therapies currently in use operate under a “one-size-fits-all” assumption, which fails to account for these biological differences. According to Zeidan, this approach often results in treatments that are less effective for women.
The study suggests that non-opioid therapies, especially those harnessing mindfulness and other meditation techniques, may be particularly beneficial for women. Because women rely on non-opioid pathways, they could achieve better pain relief from treatments that engage alternative systems rather than those dependent on the opioid system. Mindfulness meditation, which has been shown to provide effective pain relief in both men and women, is one such promising therapy. Additionally, therapies focusing on cognitive and behavioral approaches may offer further benefits, as these methods can also bypass the opioid system.
For men, traditional opioid therapies may still offer substantial relief, as men’s pain relief is more directly mediated through the endogenous opioid system. However, even for men, incorporating meditation practices could provide complementary pain relief, reducing the need for high doses of opioid medications.
This approach could be particularly useful for those suffering from chronic pain, as reliance solely on opioid medications often leads to tolerance, requiring even higher doses to achieve the same effect.
While the study provides new insights, researchers caution that more investigation is needed. Future studies should aim to confirm and expand these findings by exploring other pain relief strategies and further analyzing how the opioid and non-opioid pathways interact in the brain. This continued research could open doors to a range of non-opioid therapies that may offer safe, effective pain relief across both sexes without the high risks of addiction.
The study adds to a growing body of evidence suggesting that sex-specific approaches to pain management could help optimize patient outcomes and reduce the opioid burden, which has taken the lives of over a million Americans since 1999. As the understanding of pain mechanisms deepens, these findings underscore the importance of taking biological differences into account to create a more equitable and effective healthcare system.