In a study published in Nature on Aug. 23, researchers at the University of California, San Francisco and the University of California, Berkeley developed a device that restores communication in paralyzed patients unable to speak. The technology, which includes the use of surgically implanted electrodes and a digital avatar, is a breakthrough in the fields of artificial intelligence, neural engineering and medicine.
Ann Johnson, a 48-year-old paralysis patient, suffered from a stroke 18 years ago that led to total loss of control of her muscles. She became immobile and could no longer speak. Seeking to restore speech, she joined the researchers’ study in trying to treat her condition.
Spearheaded by Dr. Edward Chang, M.D., the Chairman of the Department of Neurological Surgery at UCSF, the study involved creating a speech-decoding system that could understand what Johnson was trying to say using electrocorticography or ECoG – an electrophysiological technique used to record electrical activity from the cerebral cortex – an AI that could predict her words and voice them through a digital avatar.
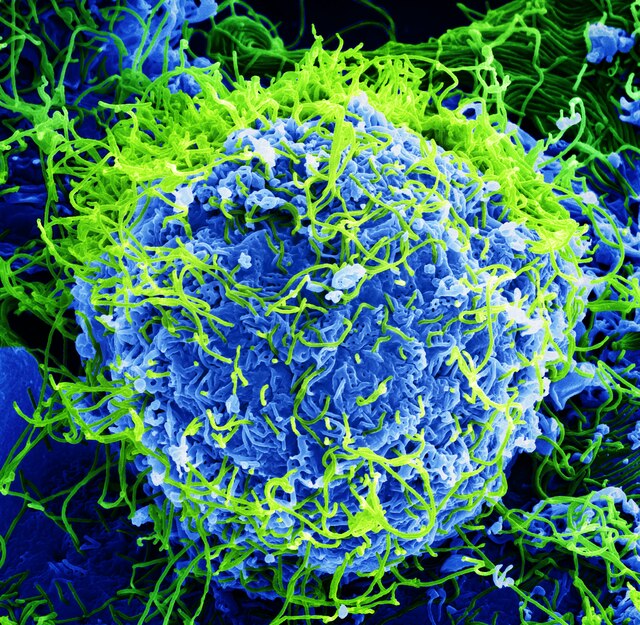
The ECoG device was composed of electrodes and was surgically implanted into Johnson’s cerebral cortex. These electrodes displayed activity whenever Johnson was making certain movements with her jaw, lips, and tongue – structures typically used for speech.
Using this neural activity, the researchers then trained machine learning models that could predict what Johnson was trying to say, generate sounds matching her intended speech and then broadcast those messages through a digital avatar, ultimately allowing her to communicate.
After participating in the study, Johnson felt a renewed sense of purpose in her life and her day-to-day life improved.
“Being a part of this study has given me a sense of purpose, I feel like I am contributing to society,” Johnson said. “It’s amazing I have lived this long; this study has allowed me to really live while I’m still alive!”
This study, like many that have been published in the past few years, illustrates AI’s burgeoning impact on the fields of medicine and science.
With the power of AI, researchers and clinicians alike can develop more targeted treatments for patients suffering hard-to-treat, sometimes even treatment-resistant, conditions.
In the case of Johnson, AI allowed her to communicate in a manner that had never been done before. In other cases, such as patients suffering from Parkinson’s disease or cortical blindness, AI can lead to the development of treatments that reduce pain or improve quality of life.
Despite AI’s revolutionary potential, it is not without flaws. In particular, in the field of radiology, AI can have devastating consequences if it goes unchecked.
According to Dr. Dan Sperling, M.D., Medical Director at the Sperling Prostate Center, he has “yet to find an AI model that has been trained on empathy, compassion, and that intangible, mysterious human capability [called] intuition.”
“AI may provide valuable information, but if I feel it necessary in any given situation, I will not hesitate to override it,” Sperling added.
At least in medicine, AI cannot be a proper substitute for humans and that many who may rely on AI remain cautious of it.
While many see the potential of AI changing the future and have already acknowledged AI’s many breakthroughs, it is important to note that it is a developing field and has a long way to go before it becomes fully established into society.